When College Students Want Mental Health Help but Get Stuck Waiting in Line
Credit to Author: Reid Champlin| Date: Wed, 16 Oct 2019 21:35:00 +0000
Rebecca King can’t remember exactly what happened the day she overdosed, in spring 2015. But she remembers well the three months beforehand: the days her anxiety confined her to her dorm, the nights destroyed by nightmares, the endless barrage of thoughts that consumed her.
The sophomore at Northeastern University was spending her spring semester doing a co-op program at Massachusetts General Hospital, her dream of becoming a nurse beginning to become reality. But as she tended to the physical ailments of her patients, her own mental health was crumbling. Away from her parents and friends, thrown into the frenetic life of professional medicine, and alone with her thoughts, she became plagued by reminders of trauma all too recent.
It had been a little over two years since one of the largest school shootings in American history had rocked her hometown of Newtown, Connecticut.
“I knew a couple of kids that passed,” King, who requested a pseudonym to protect her privacy, said. “Pretty much everyone was affected.”
Four months later, King’s father was among the six Newtown Strong members running in the 2013 Boston Marathon, each of the 26 miles dedicated to a victim of the shooting. She and her sister had been waiting for him near the finish line, and they were all close to the explosion when the bombs went off, killing three and injuring 264. While her father was unharmed, having already completed the race, the burden of bearing witness to two of America’s greatest recent tragedies weighed heavy on her mind.
“These two incidents compounded really took their toll on me,” King said. “I was having PTSD [post-traumatic stress disorder] symptoms that were interfering with my schoolwork. I was having difficulty concentrating, nightmares, intrusive thoughts.”
She knew she needed help, and thought she knew where to turn for it: the university’s Health and Counseling Services center. So she called them, hoping she could see a psychiatrist who could guide her through her trauma.
Instead, she recalls being told to wait about six weeks before she could see anyone at all.
While you might hope that King’s experience is unusual, it’s chillingly normal. Years of public efforts towards encouraging young people to seek help for their mental health concerns has paid off—a generation of college-age kids is unprecedentedly candid about suffering from mental illness. But the institutions they’re attending aren’t equipped to meet the demand. Amid a historic increase in students seeking counseling services, many people find themselves trapped on extensive waitlists, forced to endure long periods without help as centers try to meet the needs of an openly struggling generation.

More than 160 colleges and universities had waiting lists for counseling services during the 2017-2018 academic year, according to a report from the Association for University and College Counseling Center Directors (AUCCCD). On average, students at these universities waited more than three weeks just for initial appointments, and their delays didn’t end there: Students often waited just as long or longer for subsequent sessions. Many waited far longer; a VICE survey of students at 77 colleges and universities across the country found that they often waited five, six, or even ten weeks just for initial appointments.
Only a third of AUCCCD respondents reported having waitlists, but a 2017 report by Stat News found that they were present at some of the largest and most prestigious schools in the nation: the massive state universities of Michigan, Florida, and Indiana, and the world-renowned private institutions of Harvard, Columbia, and MIT. And it’s not just prominent universities that are feeling the strain of overwhelming student demand. Small liberal arts schools like Minnesota’s Carleton College and Jesuit universities like Nebraska’s Creighton also have wait times stretching weeks.
VICE contacted more than 100 schools asking for information regarding waitlists for the 2018-2019 academic year and did not receive enough responses to reach a representative average. Many schools offered minimal information or didn’t respond at all.
Being forced to wait for mental health care can have devastating consequences. King learned that the hard way. After repeated attempts to get help at Northeastern’s counseling center only to find herself languishing on the waiting list each time, she gave up on seeking help for her worsening anxiety and PTSD.
“The three months before my hospitalization were awful, the absolute darkest point in my life,” she said. She spiraled into a deeper and darker state of mind, the unbearable weight of unwanted thoughts and nightmares intensifying until she was reduced to going through the motions of life, divorced from any sense of normalcy. She remembers little about the month of April 2015, or the day she ended up overdosing, but she recalls waking up in the hospital afterwards, and being held for psychiatric treatment for several days—a period she described as being “incredibly helpful” and a turning point in her struggle. Suddenly, Northeastern took notice; she was cleared to see a psychiatrist two days after she was released.
“I really do think I ended up in the hospital because Northeastern didn’t make an effort," King said. "I expended so much energy in trying to get someone to listen to me, and they just didn’t do it. They didn’t care until I ended up in the hospital.” (VICE contacted Northeastern’s press department for comment, and the office declined to comment on both King's case and the question of wait times more generally.)
King’s story illustrates how extended periods without help can allow students’ conditions to worsen as they wait for help. A 2015 study by the National Academy of Sciences found that increased waiting times for healthcare services of any kind were linked to notedly worsened health outcomes and patient satisfaction, but the detrimental effects of waiting for mental health services are particularly worrisome.
According to a summary of the findings, “Reducing wait times for mental health services is particularly critical, because the longer a patient waits for such services, the greater the likelihood that the patient will miss the appointment.”
The risks don’t end there. Many students in VICE’s survey reported struggling academically, their grades and scholarly pursuits lagging behind as they struggle to cope.
When Jessica Kolbe was a freshman at the University of Michigan, she tried to book an appointment with an on-campus counselor as her anxiety began to spiral beyond her control. After a brief 20-minute consultation with an on-call counselor, Kolbe was told the soonest she could begin counseling was a month and a half later. But by the time she showed up for her appointment, her anxiety had become debilitating, an all-consuming state of unrest that had come to control every aspect of her life.
“My grades really plummeted. I stopped eating because I was too anxious to go to the dining hall with everybody else. I didn’t know how to cope with this constant anxiety, and whenever I would feel anxious I would have a panic attack.”
She continued to see the counselor, but after five meetings spaced between two and three weeks apart, she was cut off—the university typically only allows students a handful of sessions, and it seemed she had exhausted hers. She continued to spiral, the anxiety becoming a brutal cycle of panic attacks she couldn’t escape. She was hospitalized as her freshman year closed, and while she has improved dramatically in the two years since then, she remains frustrated with the university's counseling center.
In response to VICE’s reporting, the University of Michigan provided this statement: “We take our students' mental wellbeing very seriously, and all Counseling and Psychological Services employees are working hard to see everyone who has requested an appointment as soon as possible.”
Aaron Krasnow, associate vice president and director of counseling services at Arizona State University, knows the costs of waiting. “When you cross the threshold from identifying that you have a concern and then seeking help for it, you need, in that moment, an immediately responsive environment,” he said. “And when you don’t get that, you will not be validated for the choice that you made for help-seeking. The second thing, particularly in the lives of students, is that you lose time. And so all of the issues that affect student mental health are going to affect their academic and personal experience.”
Many students VICE spoke to expressed frustration with their counseling centers as a result of the extensive waiting times. A majority said that being told to wait weeks or months after working up the courage to ask for help led them to believe the university either didn’t care about their mental health or, worse, that they didn’t have the resources to help them at all.
Claire Connors, a junior at the College of William & Mary, said, “I think the difficulty in access has a really negative effect on the student body’s mental health. People hear horror stories about wait times and therefore are hesitant to reach out, even if they would really benefit from counseling or are in crisis. [Editor’s note: The author of this story currently attends the College of William & Mary but did not previously know Connors.]
When contacted for comment, William & Mary’s associate vice president for health & wellness Kelly Crace said that many students are able to have urgent concerns addressed same-day and that the university has a hybrid care model to handle complex challenges.
Leah Moyers, then a sophomore at Temple University, said, “The waiting period has discouraged me from seeking help, and I think it's having a poor overall effect on the student body's mental health.”
Kolbe herself told VICE, “A lot of my other friends have mental illnesses; they tried to go there and they just can’t. Everybody gives up.”

The precipitous rise in mental-health-service waitlists at universities across the U.S. is, by now, widely known. Student demand for counseling services dramatically exceeds counseling centers’ supply of mental health professionals, resources, and time needed to facilitate the process of ongoing counseling.
Students stuck on these lists are speaking up and calling for widespread reform at counseling centers across the nation. A 2017 petition demanding increased resources and expanded services from counseling centers was sent to 20 of the nation’s top universities, including Harvard, Yale, Columbia, MIT, and more, garnering nearly a thousand signatures.
Data from the Center for Collegiate Mental Health’s 2015 annual report show that over the five-year period between 2010 and 2015, the number of appointments attended increased by 38.4 percent, outpacing enrollment growth by nearly six times. This enormous growth in utilization rates has been accompanied by similarly shocking growth in students reporting mental health concerns.
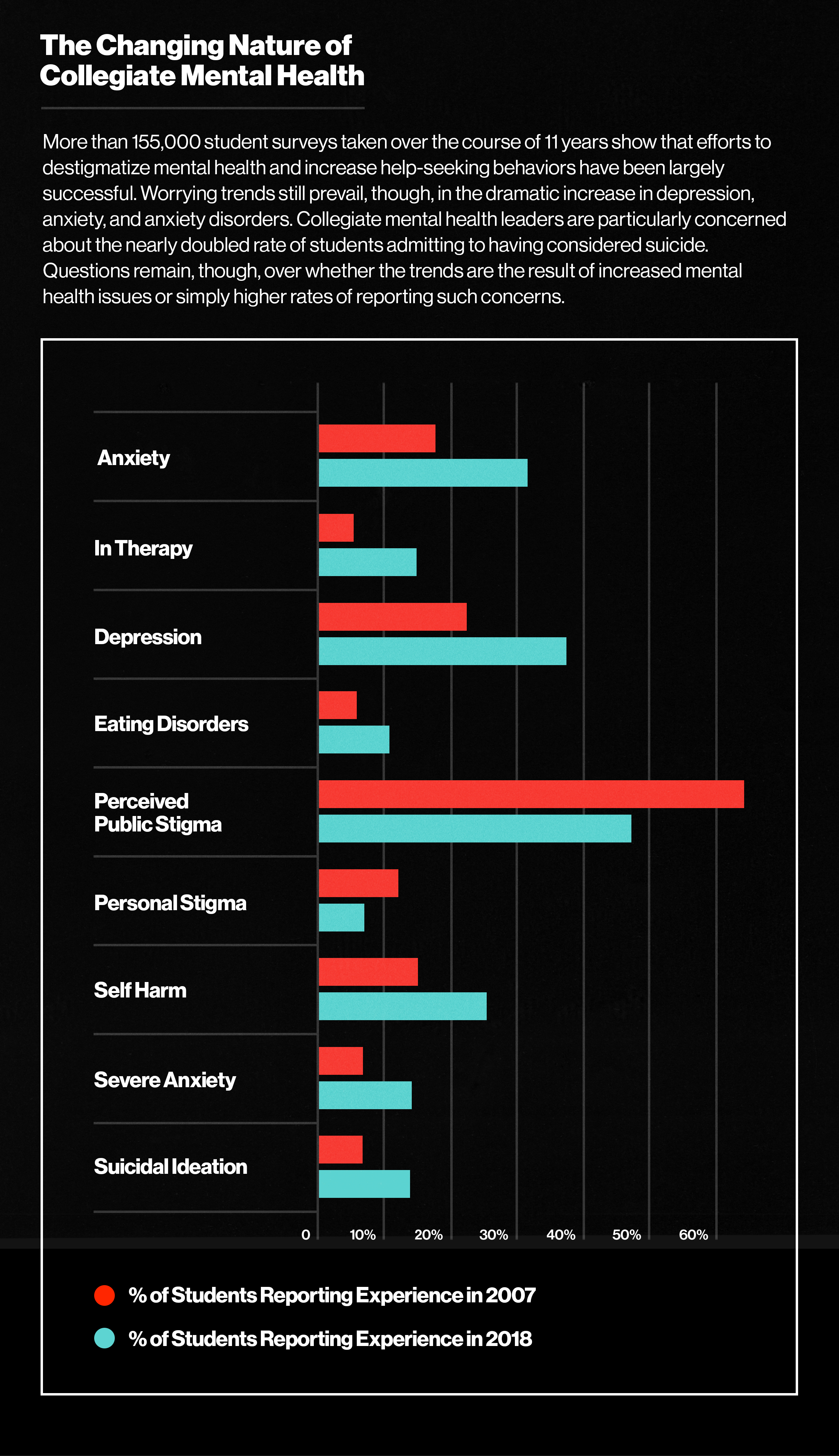
Recent studies have suggested that there are increasing rates of anxiety and depression in young people, and that teens and people in their 20s are more anxious and depressed than any generation before them. Yet many of the experts who spoke to VICE for this story suggested otherwise. In his experience, college students are not becoming less resilient or more susceptible to mental illness, said Ben Locke, executive director of Counseling and Psychological Services and director of the Center for Collegiate Mental Health (CCMH) at Penn State. Locke says that the dramatic rise of reported mental health concerns is instead the result of decades of efforts by public and private organizations to increase the visibility of mental health issues and decrease the negative stigma associated with seeking professional help.
“All of [these organizations] have been trying to convince people to seek help for mental health concerns,” Locke said. “So the fact that we’re actually seeing a dramatic increase in people seeking mental health services is completely in line with the goals of these efforts.”
Peter LeViness, director of Counseling and Psychological Services at the University of Richmond, agreed, saying, “It’s not that students are wimpy. It’s that when they are anxious or depressed or have relationship issues or when they’re having trouble adjusting, they’re much more likely to think of going to the counseling center than any previous generation would have.”
The fact that modern students are more informed about mental health issues and empowered to seek out counseling is itself a triumph. But this victory is in vain if students can’t actually access the services without significant hassle and delay, and while student utilization rates have risen precipitously over the past ten years, most counseling centers’ operating budgets have remained flat.
In every year between 2010 and 2016, the number of AUCCCD respondents that reported that their operating budgets remained constant was nearly double the number of centers that saw operating budgets increase. What's more, many schools that have managed to increase staff are nonetheless unable to increase their ability to meet student demand. Without institutional changes and money coming for expanded access and programs, the increased workforce can’t keep up with demand.
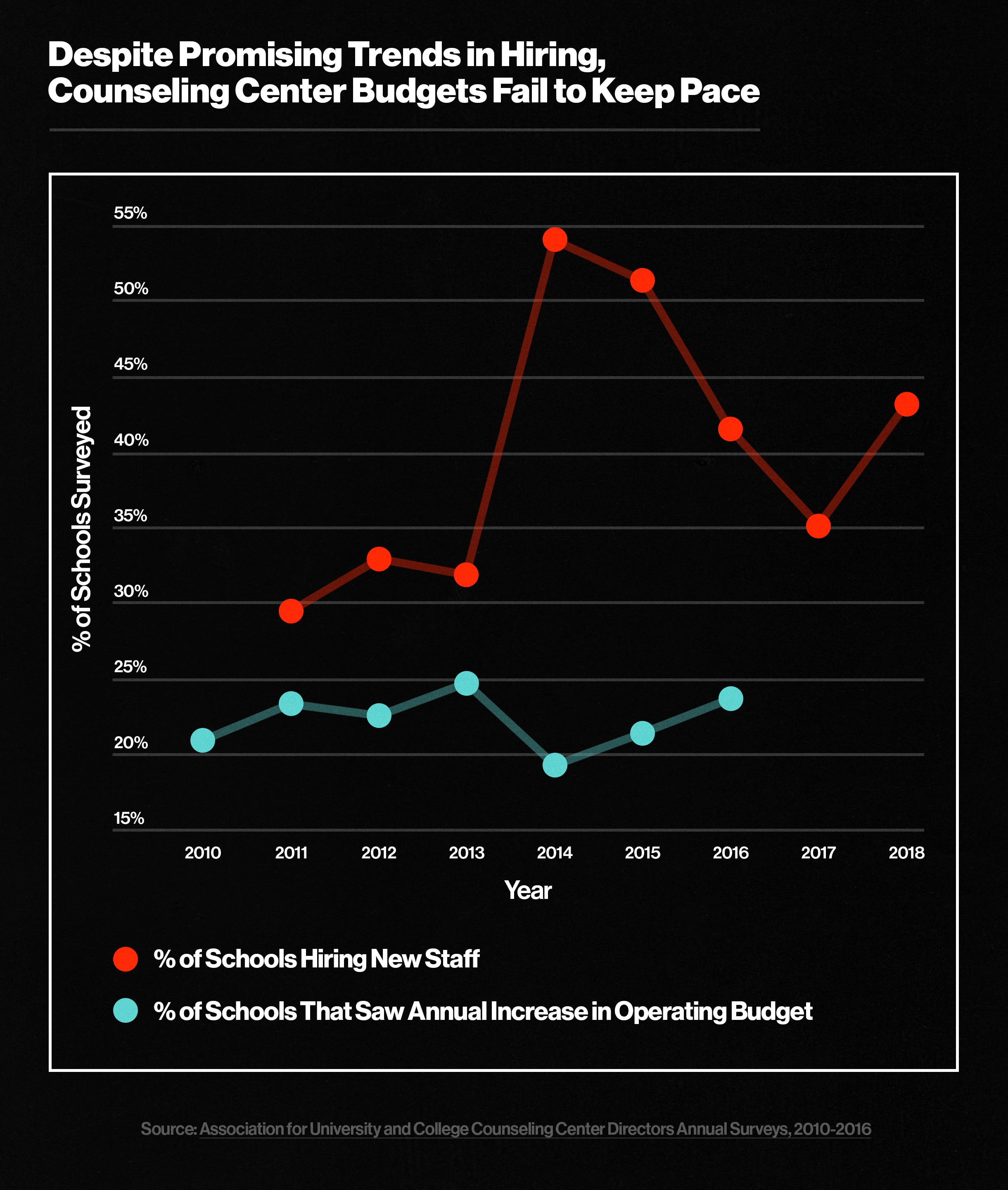
These trends come amidst a decade of decreasing state funding for public universities, with at least 45 states investing less in collegiate education in 2018 than in 2008, even though state revenues have rebounded following the recession. As universities raise tuition, cut faculty, and pursue other cost-saving expenses, counseling centers often cannot attain the additional resources they need to treat more and more students.
Any solution to the national waiting period problem must include additional resources for counseling centers in order to keep pace with the steady growth of students seeking mental health services. This singular theme, this overarching need for the resources to handle increased demand, was reflected in every interview VICE conducted on this topic.
When asked what universities would need to eliminate or reduce waitlists, Locke had a simple answer: “Resources and space. If you want to increase the ability for students to receive mental health treatment, then you’re adding resources and providing spaces for those resources to work.”
Locke and other counselors pointed to the aforementioned data showing the tepid increase in counseling-center staffing and resources compared to the meteoric rise of students seeking help, saying that the waiting periods are unlikely to decrease until universities match the supply of staff with the demands of students.
But, as state education budgets remain constrained and calls for additional resources go unheeded, many directors are trying to balance long-term counseling needs with urgent counseling needs, and, in the process, considering what the role of a counseling center itself should be.
As LeViness told VICE, “When demand exceeds capacity, you have to come up with something creative. That’s not necessarily ideal.”
At the University of Richmond, LeViness and his team have looked to balance the needs of students presenting urgent concerns with the long-term mission of providing ongoing counseling. With limited hands and limited cash, centers are having to choose what, and whom, they should focus their limited efforts on.
For LeViness, the original focus was on ensuring that students who sought out the counseling center’s assistance would be treated until they recovered, prioritizing long-term therapy appointments over immediate access. But when the waitlist ballooned to 119 people, the office shifted priorities, converting 25 counseling slots from ongoing care to quick visitation for faster access. While the waitlist has decreased, it remains stubbornly hard to eliminate, and the center now has less capacity for ongoing care.
“That’s the trade-off: do we focus on quick access or adequate care? Without more resources, I can’t do both of those well,” LeViness said.
A 2017 article by Inside Higher Education found similar trends on a national level: Since 2011, centers had increased the number of “rapid-access” service hours per student by 28 percent, simultaneously decreasing routine counseling hours by 7.6 percent.
While the experts VICE spoke to seemed to agree that additional resources would alleviate the issue, some doubted that increasing funds or staff could completely solve it.
“There’s no way to staff your way out of this challenge,” the University of Arizona’s Krasnow said. “Even if you had unlimited resources, that would presume that the counseling center was the solution path for everybody’s depression or anxiety, which is not how you want to approach a human issue.”
According to Krasnow, the entire university has a role to play in addressing mental health concerns. Many students present symptoms of anxiety related to financing their education or struggling academically, concerns that are better handled by creating an open line of dialogue with the bursar’s office or academic enrichment programs. Under his leadership, Arizona State eliminated waitlists in part by integrating the counseling center with offices across campus. In his view, in order to address the needs and concerns of the whole person, the counseling center has to engage with the whole university, bringing in physical and social well-being as important factors in alleviating the burden on the counseling center—and helping students find what will work best for them.
“The need is great, but if everybody takes responsibility—if advising and faculty themselves recognize that they play a role in the students’ well-being, then ultimately we’re a part of a much larger ecosystem as opposed to just a service delivery unit,” Krasnow said.
ASU also adopted an open-access system in which students don’t have to triage themselves or describe the urgency of their need. Despite being a campus of more than 40,000 students, patients can be seen the same day they reach out to the office due to an institutional design that allows clinicians time to treat new clients and not fill their caseloads months in advance.
The University of Pennsylvania achieved similar success in early 2019, cutting wait times from 12 to 6 days by maximizing times for initial assessments and skipping the triage phase of assessment. Other prominent programs are introducing similar institutional changes. Columbia University, for example, increased “drop-in” hours to 75 from 50 and introduced a two-pathway system of care, with “drop-in” hours tailored to addressing short-term concerns and another geared towards immediate-crisis appointments.
King is now a postgraduate at Northeastern, her mental health vastly improved since her hospitalization and subsequent counseling outside the university. But for millions of other students still seeking help at university counseling centers across the country, the waiting game continues.
If you or someone you know is experiencing thoughts of suicide, please contact the National Suicide Prevention Lifeline at 1-800-273-TALK (8255) or the Suicide Crisis Line at 1-800-783-2433.
Reid Champlin is a junior at the College of William & Mary. He reported this story as part of VICE's 2019 Collegiate Reporting Fellowship.
This article originally appeared on VICE US.